What the Midwife Heard
by www.themidwifenextdoor.com
I am always saddened when I hear a woman tell me about her birth plans, and then say, “My doctor said he’ll go along with whatever I want as long as it is safe”. Nine times out of ten, that woman is coming back to me later to talk about what went wrong and wonder why her doctor didn’t come through for her.
As someone on the inside of the circle of modern obstetrics, I am privy to a lot of conversation that reveals to me where OB providers are really coming from. Many put on a good face, and reassure their patients that they only have the patient’s best interest at heart and would never do anything that wasn’t necessary for the mother or baby’s safety. I believe that many of the providers sincerely mean what they are saying. The problem is that they do not keep current on the literature, and when evidence is provided that indicates lack of support for a routine intervention, they rely on their personal experience and the fact that they’ve not often seen complications from their interventions, to justify continuing the way they always have. Ladies, it is so important to discuss with your provider his or her c-section rate, definition of normal birth, how often they see a normal birth, and what interventions they do routinely. You cannot count on your provider’s personality, bedside manner, or promises of only intervening when necessary for safety, because they s/he may not know that there are safe alternatives to routine interventions much of the time, and may believe the intervention is being done for your safety. One has only to look at the very high c-section rate in our country to understand this mentality.
With this said, I would like to share some comments overheard in the doctor’s lounge and at the nurse’s station over the last few days. I share these not to disparage physicians and nurses, but to help women understand that what you are hearing from your doctor’s lips very likely is not what he or she is saying behind your back.
Physician: “She’ll never get this baby out vaginally, but she needs to feel like she’s had a fair chance, so let’s ‘pit to distress’. We can get it over with in a couple of hours, and she’ll feel like she had a good shot at it.” (Spoken of a woman with a suspected 9 pound baby, that ended out weighing 7 lbs.)
Nurse (speaking to midwife about a the midwife trying to induce with as little interventions as possible): “I’m not going to turn the pitocin on unless you put in internal monitors. She can just sit here all day, but you can’t make me do it without internals if I don’t feel safe”.
Physician (When nurse pointed out to him that his chosen treatment for the patient was not evidence-based): “Well, that’s why it’s good to be a dinosaur sometimes. You don’t have to worry about what the evidence says!”
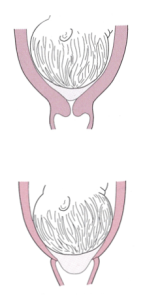
Physician: “You need to lie on your back to deliver the baby in case the shoulders get stuck” (evidence shows this is the one position that makes it most likely the shoulders will get stuck).
Physician: “Don’t feel bad about having a c-section. Think of it this way, you’ll be in good company with all the celebrities who have pretty vaginas!”
Physician (one reputed to have a great personality and be willing to accomodate mother’s wishes, spoken to parents when they asked him about second opinion regarding his recommendation for immediate induction): “I am very uncomfortable being questioned like this. If you don’t trust my judgement, you can find yourself another provider–that is, if anyone will take you at 39 weeks!”
Nurse: “We’re admitting another one of those hypnobirthers. Make her stay on the monitor so she can’t get out of bed, and she’ll agree to the epidural by the time she’s three centimeters!”
Physician: “She (the patient) didn’t want to take my advice, so she deserves whatever happens to her.”
Physician (trying to get mother to sign a consent for c-section for failure to progress satisfactorily in two hours): “Sure, we can wait longer if that’s what you want. Personally, I think it would be better to head back to the OR at a leisurely pace rather than waiting until your baby takes a nosedive and we have to run you back there.” Mother then asked him if the baby was having any distress. Physician answered: “No, but do you want to wait until he does? Do you really want to put your baby through that stress? Birth is dangerous and stressful for babies!”
Physician (spoken to patient handing him a written birth plan): “Oh, you don’t really want a birth plan, do you? Every patient I have who writes a birth plan ends up with a c-section. It’s a prescription for trouble. Besides, that’s why you’re paying me to make the decisions. I’ve been to 8 years of school to learn how to safely manage labors. Do you really think you know more than I do just because you’ve read a website on birth plans?”
Physician (to a patient who was expressing discomfort over a vaginal exam): “Come on, now, you’ve had something a lot bigger than my finger in there! How’d you ever manage to get pregnant if you can’t put up with this?”
Birth Sense Tip: Pay attention to your intution. If your physician seems impatient with your questions, patronizing in any way, or unable to describe any of the ways s/he supports normal birth, RUN, don’t walk, for the exit and find another provider. Don’t just hope that things will work out OK, because chances are your physician is saying things like the comments above, about YOU, behind your back.